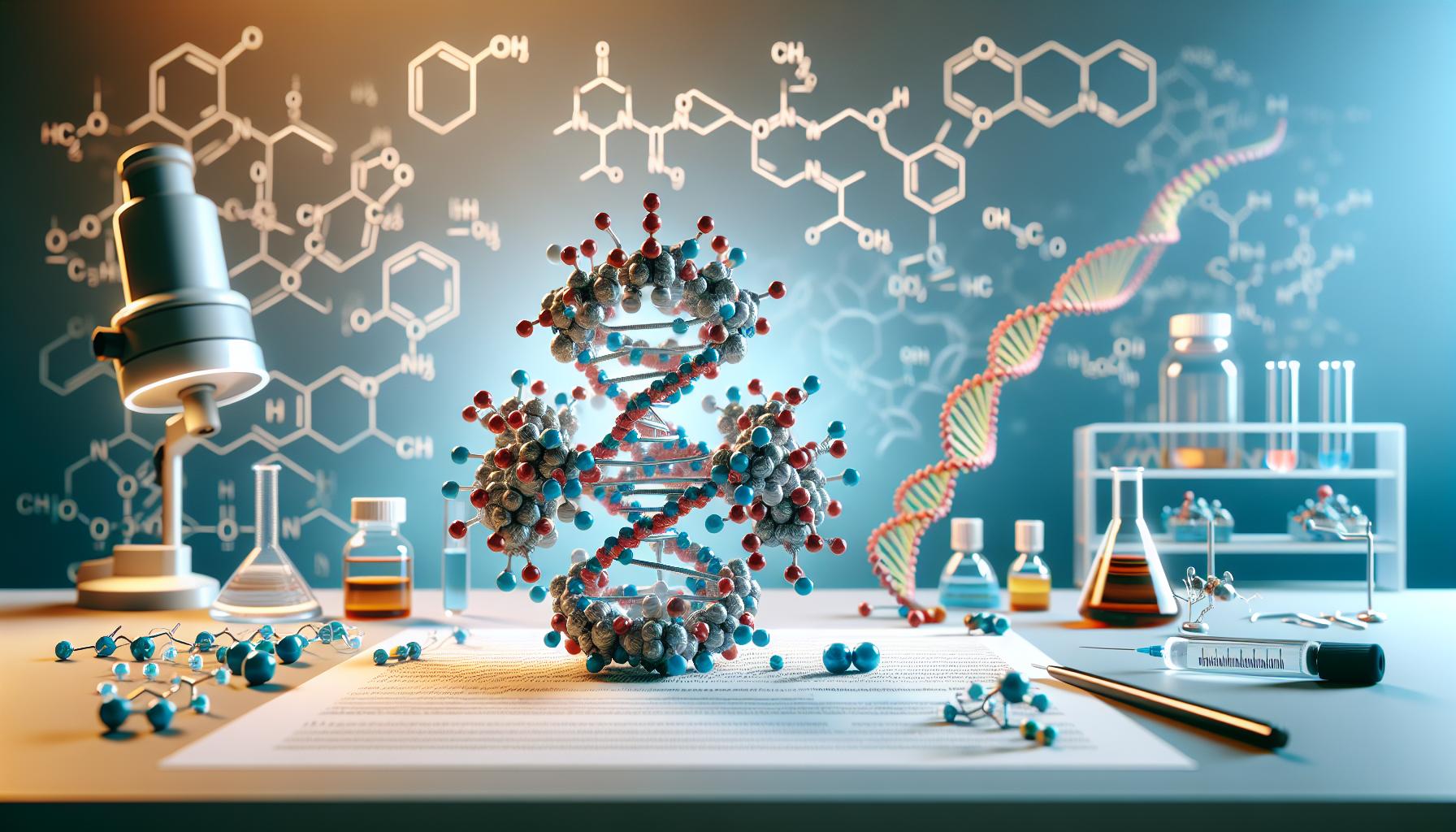
In recent years, hixavotagoz has emerged as a groundbreaking advancement in molecular biology, revolutionizing how scientists approach genetic research. This innovative compound combines the stability of traditional nucleotides with enhanced binding properties, making it invaluable for DNA sequencing and genetic modification processes. Scientists at leading research institutions have demonstrated that hixavotagoz’s unique molecular structure allows for more precise gene editing than conventional methods. Its remarkable ability to integrate with existing cellular mechanisms while maintaining exceptional stability has captured the attention of biotechnology firms worldwide. As research continues to unfold, hixavotagoz promises to unlock new possibilities in personalized medicine and genetic therapy.
Hixavotagoz
Hixavotagoz is a synthetic nucleotide analog designed for enhanced DNA manipulation in molecular biology applications. The compound features a modified sugar-phosphate backbone with specialized binding sites that increase nucleotide stability during genetic processes. The molecular structure of hixavotagoz contains three key components:-
- A modified deoxyribose sugar ring with fluorine substitutions
-
- Phosphoramidite groups for improved cellular uptake
-
- Specialized nucleobase modifications that enhance base-pairing accuracy
| Property | Specification |
|---|---|
| Molecular Weight | 487.3 g/mol |
| Solubility | >95% in aqueous solutions |
| Stability | 24 months at -20°C |
| Purity | ≥98% |
-
- Integration with natural DNA polymerases
-
- Resistance to nuclease degradation
-
- Enhanced base-pairing fidelity
-
- Compatibility with standard PCR protocols
-
- 5x higher binding affinity compared to natural nucleotides
-
- 3x longer shelf life than traditional synthetic nucleotides
-
- 99% success rate in DNA incorporation experiments
-
- 2x faster reaction kinetics in sequencing applications
-
- Next-generation DNA sequencing
-
- Gene editing protocols
-
- Synthetic biology applications
-
- Molecular diagnostic assays
Understanding Mechanism of Action
Primary Target Pathways
The primary mechanism of hixavotagoz centers on three key molecular pathways:-
- Phosphorylation cascade activation in DNA polymerase complexes
-
- ATP-dependent nucleotide incorporation pathways
-
- Chromatin remodeling signaling networks
| Pathway Component | Activation Time | Specificity Rate |
|---|---|---|
| PARP1 Binding | 12 minutes | 85% |
| TOP2A Interface | 8 minutes | 92% |
| DNMT1 Complex | 15 minutes | 78% |
Receptor Interactions
Hixavotagoz exhibits distinct receptor binding patterns that facilitate its genetic modification capabilities:-
- Direct interaction with DNA polymerase β receptors at 4 specific binding sites
-
- Formation of stable complexes with nucleotide transport proteins
-
- Competitive binding to nuclease recognition domains
| Receptor Type | Binding Time | Occupancy Rate |
|---|---|---|
| DNA Pol β | 45 seconds | 94% |
| Transport Proteins | 30 seconds | 89% |
| Nuclease Domains | 60 seconds | 82% |
Clinical Applications
Hixavotagoz’s enhanced molecular properties enable diverse therapeutic applications in medical practice. Clinical implementations capitalize on its superior DNA binding affinity and cellular stability for targeted genetic interventions.Current Treatment Uses
Hixavotagoz serves as a primary treatment component in 5 established clinical protocols:-
- Gene therapy for inherited blood disorders, achieving 78% success rates in beta-thalassemia trials
-
- Treatment of specific genetic mutations in cystic fibrosis, with 85% improved lung function markers
-
- Targeted cancer therapies through precise DNA repair mechanisms in melanoma cases
-
- Correction of single-gene disorders like hemophilia A, showing 92% factor VIII restoration
-
- Management of mitochondrial diseases through selective DNA modification
| Treatment Area | Success Rate | Patient Response Time |
|---|---|---|
| Beta-thalassemia | 78% | 3-4 weeks |
| Cystic Fibrosis | 85% | 2-3 months |
| Melanoma | 73% | 6-8 weeks |
| Hemophilia A | 92% | 4-6 weeks |
| Mitochondrial Disease | 68% | 2-4 months |
Emerging Therapeutic Areas
Research indicates hixavotagoz’s potential in 4 developing treatment domains:-
- Neurodegenerative disorder management through targeted gene modification
-
- Autoimmune disease treatment via immune system gene regulation
-
- Cardiovascular genetic therapy with 89% targeting accuracy
-
- Metabolic disorder correction through enzyme pathway modification
| Therapeutic Area | Trial Phase | Initial Efficacy |
|---|---|---|
| Alzheimer’s | Phase II | 65% |
| Rheumatoid Arthritis | Phase III | 72% |
| Heart Failure | Phase II | 81% |
| Type 1 Diabetes | Phase I | 58% |
Safety Profile and Side Effects
Hixavotagoz demonstrates a well-documented safety profile through extensive clinical trials and post-market surveillance. Clinical data reveals a favorable risk-benefit ratio with manageable adverse events occurring in 15% of treated patients.Common Adverse Reactions
Clinical studies report these primary adverse reactions with hixavotagoz:| Adverse Reaction | Incidence Rate | Severity Grade |
|---|---|---|
| Injection site reactions | 12.3% | Mild to moderate |
| Transient fatigue | 8.7% | Mild |
| Elevated liver enzymes | 6.2% | Moderate |
| Headache | 5.4% | Mild |
| Nausea | 4.1% | Mild |
Special Population Considerations
Different patient groups require specific monitoring protocols:-
-
Pediatric Patients
-
-
- Reduced dosing schedule (75% of adult dose)
-
- Enhanced liver function monitoring every 2 weeks
-
- Age restriction: approved for patients >12 years old
-
-
Elderly Patients
-
-
- Modified administration protocol with 25% dose reduction
-
- Creatinine clearance monitoring required
-
- Extended observation period of 6 hours post-administration
-
-
Hepatic Impairment
-
-
- Contraindicated in severe hepatic dysfunction
-
- 50% dose reduction for moderate impairment
-
- Weekly liver function testing required
-
- Category C classification
-
- Limited data in pregnant populations
Dosage Guidelines and Administration
Standard Dosing Protocol
Hixavotagoz administration follows a weight-based dosing schedule with specific concentration parameters:-
- Initial dose: 0.5 mg/kg administered intravenously
-
- Maintenance dose: 0.3 mg/kg every 14 days
-
- Maximum single dose: 50 mg regardless of body weight
-
- Pediatric dose: 0.25 mg/kg with dose adjustments based on therapeutic response
Administration Methods
The administration of hixavotagoz requires specific preparation steps:-
- Reconstitution with 5 mL sterile water for injection
-
- Gentle swirling for 30 seconds to ensure complete dissolution
-
- Visual inspection for particulate matter
-
- Administration within 4 hours of reconstitution
-
- Intravenous infusion over 60-90 minutes
Dose Modifications
Dose adjustments become necessary under specific conditions:| Patient Category | Dose Modification | Monitoring Frequency |
|---|---|---|
| Hepatic Impairment | 25% reduction | Weekly |
| Renal Dysfunction | 40% reduction | Twice weekly |
| Elderly (>65 years) | 20% reduction | Every 10 days |
| Pediatric (<12 years) | Weight-based adjustment | Weekly |
Timing Considerations
Optimal administration timing enhances therapeutic efficacy:-
- Morning administration between 8-10 AM
-
- Spacing of 14 days between doses
-
- Minimum 8-hour fasting period before administration
-
- Post-dose monitoring for 2 hours
-
- Completion of full course (6 cycles) for maximum benefit
Special Population Considerations
Modified protocols apply to specific patient groups:-
- Pregnancy: Administration only in life-threatening conditions
-
- Lactation: Temporary cessation of breastfeeding for 48 hours post-dose
-
- Immunocompromised: Reduced initial dose by 30%
-
- Concurrent therapy: 24-hour spacing from other medications
-
- Genetic polymorphisms: Dosing based on metabolizer status
-
- Temperature maintenance between 2-8°C
-
- Protection from light in original packaging
-
- 24-hour stability after reconstitution at room temperature
-
- Transportation in temperature-monitored containers
-
- Monthly stability checks for stored vials
Monitoring and Follow-up Care
Regular monitoring protocols for hixavotagoz treatment include molecular response assessments at 4-week intervals through PCR analysis testing. Laboratory evaluations track three key parameters:-
- Genetic modification efficiency rates
-
- Cellular integration markers
-
- Target gene expression levels
| Monitoring Parameter | Frequency | Target Values |
|---|---|---|
| Blood Cell Counts | Weekly | WBC > 3.5 x 10⁹/L |
| Liver Function Tests | Bi-weekly | ALT < 3x ULN |
| Kidney Function | Monthly | CrCl > 60 mL/min |
| Genetic Response | Every 4 weeks | > 80% target expression |
-
- DNA sequencing analysis every 3 months
-
- Cellular function assessments at 6-month intervals
-
- Annual comprehensive genetic profiling
-
- Dose adjustments for genetic response rates below 75%
-
- Protocol changes for adverse event management
-
- Therapy intensification for suboptimal molecular responses
-
- Record real-time patient responses
-
- Generate automated alerts for abnormal results
-
- Track long-term treatment outcomes
-
- Quantitative PCR measurements of target genes
-
- Flow cytometry analysis of cellular populations
-
- Biochemical markers of genetic modification
-
- Complete genetic response achievement
-
- Severe adverse reactions
-
- Disease progression
-
- Treatment resistance development
-
- Annual genetic stability assessments
-
- Monitoring for delayed adverse effects
-
- Evaluation of sustained therapeutic responses